Curriculum
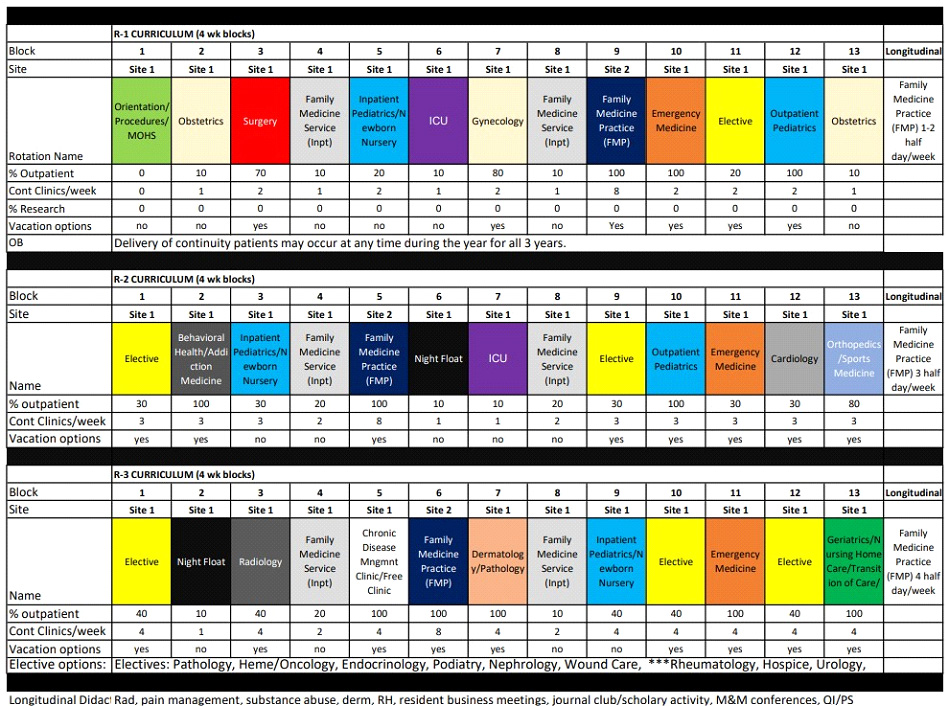
The MHFMRP curriculum has been created to give residents a strong foundation in rural settings, outpatient primary care, inpatient care, and urgent/Emergency Medicine. In addition, it allows significant time for electives and opportunities to consolidate their knowledge and apply it to rural community medicine.
All rotations will include a clear set of Goals and Objectives in compliance with the ACGME.
Family Medicine Inpatient Service Goals and Objectives
Rotation Goals and Objectives
Marion Health Family Medicine Residency Program (MHFMRP)
Last Updated 8/18/2023
Name of Rotation: Family Medicine Inpatient Rotation (FMIP)
Rotation Description: The FMIP rotation will allow the resident to evaluate and manage patients with common acute medical conditions requiring inpatient care in a compassionate, evidence-based, and culturally appropriate manner. Training will focus not only on clinical care issues but also on coordinating patient care with non-physician providers, subspecialists, and allied health professionals on patient care transitions and the spectrum of leadership, cost, quality, and performance activities within the purview of inpatient adult medicine.
The FMIP is a 4-week rotation completed twice a year by a PGY-1, PGY-2, and PGY-3. The service is run by either a Family Medicine or Internal Medicine faculty member. Admissions to the team will be (preferentially) from the FMP Resident Clinic and the FMP Faculty Clinic. The team will also rotate admissions from the ED with the hospitalist adult medicine service. Residents will manage the day-to-day care of the patients on the FMIP service. Residents will not take call during this rotation. The service is capped at 16 patients, with PGY-1 (6 patients), PGY-2(10 patients), and PGY-3 (16 patients for the service) unless the program director authorizes an increase in that number based on extraordinary circumstances.
Residents are required to attend their weekly continuity clinic or clinics. Weekly didactic sessions should be attended as time permits.
ACGME Family Medicine Residency Review Committee (RRC) Requirements:
The Family Medicine RRC requirements for this rotation (effective 2023) state that: “Residents must have at least 600 hours (or six months), and 750 patient encounters dedicated to the care of hospitalized adult patients with a broad range of ages and medical conditions.” (IV.C.3.j ).
Objectives:
Patient Care:
- PGY-1
- Acquire accurate and relevant history from the patient efficiently and accurately.
- Seek and obtain appropriate, verified, and prioritized data from secondary sources (e.g., family, records, pharmacy).
- Perform an accurate and appropriately targeted physical examination focusing on a patient’s complaints and medical conditions. Identify pertinent abnormalities using common maneuvers. (e.g., can identify grade 3 or higher cardiac murmur)
- Accurately track important changes in the physical examination over time.
- Synthesize all available data, including interviews, physical examination, and preliminary laboratory data, to define each patient’s central clinical problem.
- Develop prioritized differential diagnoses, evidence-based diagnostic, and therapeutic plans for common inpatient conditions.
- Formulate a comprehensive problem list for each patient.
- Make appropriate clinical decisions based on the results of common diagnostic testing, including but not limited to routine blood chemistries, hematologic studies, coagulation tests, arterial blood gases, electrocardiograms, chest radiographs, pulmonary function tests, and urinalysis.
- Recognize situations with a need for urgent or emergent medical care.
- Recognize when to seek additional guidance.
- With supervision, manage patients with common clinical disorders seen in inpatient adult medicine.
- PGY-2
- Obtain relevant historical subtleties that inform and prioritize differential diagnoses and diagnostic plans, including sensitive, complicated, and detailed information for which the patient may not often volunteer.
- Demonstrate and teach how to elicit important physical findings for junior healthcare team members.
- Modify problem formulation, differential diagnosis, and care plan based on the evolution of clinical data over time and evidence-based medicine.
- Make appropriate clinical decisions based on the results of more advanced diagnostic tests.
- Provide appropriate care for health maintenance and disease prevention.
- With minimal supervision, manage patients with common clinical disorders seen in inpatient general medicine.
- With supervision, manage patients with complex clinical disorders seen in inpatient general medicine.
- Provide specific, responsive consultation to other services.
- PGY-3
- Role model gathering subtle and reliable information from the patient for junior healthcare team members.
- Routinely identify subtle or unusual physical findings that influence clinical decision-making (e.g., can identify grade III cardiac murmur).
- Recognize disease presentations that deviate from common patterns and that require complex decision-making.
- Appropriately perform procedures as recommended by guidelines and provide post-procedure management.
- Consider the costs, risks, and benefits when recommending diagnostic tests.
- Initiate management and stabilize patients with emergent medical conditions.
- Manage patients with conditions that require intensive care.
- Independently manage patients with a broad spectrum of clinical disorders using evidence-based medicine, including gender-specific diseases.
- Coordinate the care of patients with complex and rare medical conditions.
- Customize care in the context of the patient’s preferences and overall health.
- Provide inpatient medicine consultations for patients.
Procedures:
- ACLS
- Abdominal paracentesis
- Arterial line placement
- Arthrocentesis
- Central line placement
- Chest Tube Placement
- Drawing arterial blood
- Drawing venous blood
- EKG interpretation
- I&D Abscess
- IV placement
- Lumbar Puncture
- NG tube placement
- Pulmonary artery catheter placement
- Thoracentesis
Medical Knowledge:
- PGY-1
- Understand the relevant pathophysiology and basic science for common medical conditions.
- Demonstrate sufficient knowledge to diagnose and treat common conditions that require hospitalization.
- Understand indications for the basic interpretation of common diagnostic testing, including but not limited to routine blood chemistries, hematologic studies, coagulation tests, arterial blood gases, ECG, chest radiographs, pulmonary function tests, urinalysis, and other body fluids.
- Accurately identify the following patterns on an EKG:
- Myocardial infarction
- Arrhythmias, including supraventricular tachycardias, atrial fibrillation and flutter, heart blocks, ventricular tachycardia, and ventricular fibrillation
- Diagnose the following conditions on X-ray and/or CT:
- Pneumonia
- Heart failure
- Chronic obstructive pulmonary disease
- Ileus
- Intestinal obstruction
- Interpret an ABG
- Interpret a PFT
- Understand the sources of medical information, research, and evidence-based guidelines and effectively utilize this information in practice.
- Develop knowledge of patient-directed information and education to enhance the patient’s understanding and management of their condition.
- PGY-2
- Demonstrate sufficient knowledge to evaluate common conditions requiring hospitalization.
- Demonstrate sufficient knowledge to diagnose and treat undifferentiated and emergent conditions.
- Demonstrate sufficient knowledge to provide health maintenance and preventive care.
- Demonstrate sufficient knowledge to identify and treat common medical conditions requiring higher acuity inpatient care.
- Understand indications for and have basic skills in interpreting more advanced diagnostic tests.
- Understand prior probability and test performance characteristics.
- PGY-3
- Demonstrate sufficient knowledge to evaluate and coordinate the care of complex medical conditions and multiple coexistent conditions.
- Demonstrate sufficient knowledge of socio-behavioral sciences, including but not limited to healthcare economics, medical ethics, and medical education.
- For all years, expected Medical Knowledge will include expertise in the diagnosis and management of:
- Abdominal Pain
- Acid-base disturbances
- ACS
- Advance directives and code status
- AFIB
- Alcohol withdrawal
- Altered Mental Status
- Anemia
- ARF
- Arrhythmias
- Asthma
- Back Pain
- Cellulitis
- Chest Pain
- CHF
- Cirrhosis
- COPD
- Decubitus Ulcers
- Diarrhea
- DM
- Edema
- Electrolyte imbalances
- Fever
- GI Bleeding
- Hemoglobinopathies
- Hepatitis
- HTN
- Nephrolithiasis
- Nutritional assessment and support
- Palliative Care
- Pancreatitis
- Pathologic Weight loss
- Pneumonia
- Polycythemia
- Preoperative risk assessment
- Preoperative risk reduction interventions
- Pronouncement of death
- Postoperative management (pain, glycemic control, antibiotics)
- Seizure
- Sepsis
- SOB
- Stroke/TIA
- Substance Abuse
- Suicidal Ideation
- Syncope
- Tylenol overdose
- VTE
Interpersonal Skill and Communication:
- PGY-1
- Engage patients/advocate in shared decision-making for uncomplicated diagnostic and therapeutic scenarios.
- Understand the patient’s expectations, goals, and opinions of their health, lifestyle, beliefs, and chronic conditions.
- Utilize patient-centered education strategies.
- Engage patients/advocates in shared decision-making for difficult, ambiguous, or controversial scenarios.
- Use an interpreter to engage patients in the clinical setting, including patient education.
- Demonstrate sensitivity to patient differences, including but not limited to race, culture, gender, sexual orientation, socio-economic status, literacy, and religious beliefs.
- Effectively communicate with other caregivers to maintain appropriate continuity during the transition of care.
- Deliver appropriate, concise oral presentations.
- Effectively communicate the plan of care to all members of the healthcare team.
- Effectively request consultative services.
- Provide legible, accurate, complete, and timely written communications congruent with medical standards.
- PGY-2
- Appropriately counsel patients about the risks and benefits of tests and procedures, highlighting cost awareness and resource allocation.
- Role-model and teach effective communication with the next caregivers during the transition of care.
- Engage in collaborative communication with all members of the healthcare team.
- Communicate the consultant’s role to the patient to support the primary care relationship.
- Ensure brief, relevant, and patient-specific written communication.
- PGY-3
- PGY-3s will role-model effective communication skills in challenging situations.
- Actively seek to understand patient differences and views, reflecting this in respectful communication and shared decision-making with the patient and the healthcare team.
- Communicate consultative recommendations to the referring team in an effective manner
Professionalism:
- PGY-1
- In all things, advocate for the patient and do the right thing.
- Document and report clinical information truthfully.
- Follow formal policies.
- Accept personal errors and acknowledge them.
- Demonstrate empathy and compassion to all.
- Demonstrate commitment to relieve suffering.
- Provide support (physical, psychological, social, and spiritual) for dying patients and their families.
- Communicate constructive feedback to other members of the healthcare team.
- Respond promptly and appropriately to clinical responsibilities, including calls and pages.
- Carry out timely interactions with colleagues, patients, and their designated caregivers.
- Recognize and manage obvious conflicts of interest, such as caring for family members and professional associates as patients.
- Recognize when it is necessary to advocate for individual patient needs.
- Dress and behave appropriately.
- Maintain appropriate professional relationships with patients, families, and staff.
- Ensure prompt completion of clinical, administrative, and curricular tasks.
- Ensure completion of results, review medical documentation, and address communications within the expected time frames.
- Recognize the scope of their abilities and ask for supervision and assistance appropriately.
- Recognize and address personal, psychological, and physical limitations affecting professional performance.
- Treat patients and coworkers with dignity, civility, and respect, regardless of race, culture, gender, ethnicity, age, or socio-economic status.
- Maintain patient confidentiality.
- Recognize that disparities exist in health care among populations and that they may impact the patient’s care.
- PGY-2
- Recognize, respond to, and report impairment of colleagues or substandard care.
- Recognize and take responsibility for situations where public health supersedes individual health (e.g., reportable infectious disease).
- Recognize the need to assist colleagues in the provision of duties.
- Educate and hold others accountable for patient confidentiality.
- PGY-3
- Uphold ethical expectations of research and scholarly activity.
- Provide leadership for a team that respects patient dignity and autonomy.
- Maintain ethical relationships with the industry.
- Recognize and manage subtler conflicts of interest.
- Effectively advocate for individual patient needs.
- Serve as a professional role model for more junior colleagues (e.g., medical students and interns).
- Recognize and manage conflict when patient values differ from their own.
- Embrace physicians’ role in assisting the public and policymakers in understanding and addressing causes of disparity in disease and suffering.
- Advocate for appropriate allocation of limited health care resources.
Practice-Based Learning and Improvement:
- PGY-1
- Identify areas in the resident’s own practice and local system that can be changed to improve processes and outcomes of care.
- Identify learning needs (clinical questions) as they emerge in patient care activities.
- Access medical information resources to answer clinical questions and library resources to support decision-making.
- With assistance, appraise clinical research papers’ validity, importance, and applicability.
- Determine if clinical evidence can be generalized to an individual patient.
- Respond welcomingly and productively to feedback from all healthcare team members, including faculty, peer residents, students, nurses, allied health workers, patients, and their advocates.
- Actively seek feedback from all members of the healthcare team.
- Actively participate in teaching conferences.
- Engage in quality improvement activities.
- PGY-2
- Classify and precisely articulate clinical questions.
- Develop a system to track, pursue, and reflect on clinical questions.
- Effectively and efficiently search databases for original clinical research articles.
- Effectively and efficiently search evidence-based summary medical information resources.
- With assistance, appraise clinical guideline recommendations.
- Reflect on feedback in developing personal improvement plans.
- Maintain awareness of the situation and respond to meet situational needs.
- Integrate teaching, feedback, and evaluation with supervision of interns’ and students’ patient care.
- Engage in quality improvement intervention.
- PGY-3
- Engage in quality improvement intervention.
- Appraise the quality of medical information resources and select among them based on the characteristics of the clinical question.
- Customize clinical evidence for an individual patient.
- Communicate the risks and benefits of alternatives to patients.
- Integrate clinical evidence, clinical context, and patient preferences into decision-making.
- Calibrate self-assessment with feedback and other external data.
- Reflect (during the event) when surprised, apply new insights to future clinical scenarios, and reflect (on the action) back on the process.
- Take a leadership role in the education of all members of the healthcare team.
Systems-Based Practice:
- PGY-1
- Understand the unique roles and services provided by local healthcare delivery systems.
- Appreciate the roles of a variety of health care providers, including, but not limited to, consultants, therapists, nurses, home care workers, pharmacists, and social workers.
- Work effectively as a member of the interprofessional team to ensure safe patient care.
- Consider alternative solutions provided by other teammates.
- Recognize system issues that increase the risk for error, including barriers to optimal patient care.
- Reflect an awareness of common socio-economic barriers that impact patient care.
- Minimize unnecessary care, including tests, procedures, therapies, and ambulatory or hospital encounters.
- PGY-2
- Manage and coordinate care and care transitions across multiple healthcare settings, including ambulatory, subacute, acute rehabilitation, and skilled nursing.
- Identify, reflect upon, and learn from critical incidents such as near misses and preventable medical errors.
- Dialogue with care team members to identify risks for and prevent medical errors.
- Understand how cost-benefit analysis is applied to patient care (i.e., via principles of screening tests and the development of clinical guidelines).
- Identify costs for common diagnostic or therapeutic tests.
- Demonstrate the incorporation of cost-awareness principles into standard clinical judgments and decision-making.
- PGY-3
- Negotiate patient-centered care among multiple care providers.
- Demonstrate how to manage the team by utilizing the skills and coordinating the activities of interprofessional team members.
- Understand mechanisms for analysis and correction of system errors.
- Demonstrate ability to understand and engage in a system-level quality improvement intervention.
- Partner with other healthcare professionals to identify and propose improvement opportunities within the system.
- Identify the role of various healthcare stakeholders, including providers, suppliers, financiers, purchasers, and consumers, and their varied impact on the cost and access to healthcare.
- Understand coding and reimbursement principles.
- Demonstrate the incorporation of cost-awareness principles into complex clinical scenarios.
Teaching Methods:
- The resident will gain knowledge of common inpatient medicine problems through one-on-one discussion and precepting with the attending physician, teaching rounds, and independent reading.
- The resident will also employ case-based scenarios and simulations to reinforce knowledge.
- The resident will be expected to develop teaching skills through participating in the teaching of medical students and junior residents in the inpatient setting.
Supervision:
Supervised patient care in the hospital:
- Residents will initially be directly observed with patients to facilitate the acquisition of excellent history-taking, physical exams, and procedural skills.
- As residents become more proficient, they will interact independently with patients and present cases to faculty:
- For PGY-1s, the initial emphasis will be on diagnosis and basic management.
- For more senior residents, the focus will be on medical decision-making, and residents will work with supervising physicians to finalize a care plan.
Evaluation:
- Case and procedure logs
- Mini-CEX bedside evaluation tool
- 360 Evaluation
- Verbal mid-rotation individual feedback
- An attending written evaluation of the resident at the end of the month based on rotation observations and chart review.
